-
Written by Dr.Mehmet Demircioglu
- Estimated Reading Time 8 Minutes
Shedding of Transplanted Hair or Permanent Loss of Hair Grafts in the Initial Months Following a Hair Transplant
The initial 2-3 months following hair transplant surgery are crucial for patients, marked by a common concern, the nature of hair shedding during this period.
This is a transitional phase where the scalp adjusts to the new grafts, and understanding this process is essential for setting realistic expectations for patients. This phase often raises questions and anxieties about the success and outcomes of the procedure.
Recently, a hair transplant patient contacted Diamond Hair Clinic‘s WhatsApp line to seek consultation regarding an issue they faced post-surgery. Almost 2.5 months ago, the patient underwent DHI (Direct Hair Implantation) procedure at a hair transplant clinic in Turkey, not at our clinic.
This context is essential, as it highlights the variety of experiences and results patients may encounter depending on where they receive treatment, especially in the context of Turkey’s hair transplant industry, which is known for its different quality range of clinics.
So, in this case, there might be concerns about the quality of the hair transplant surgery, particularly the placement of the graft to the scalp, which could significantly impact graft survival.
The clinic where the patient underwent hair transplant surgery can be considered one of the hundreds of low-cost Turkish hair mills, operating 20-30 patients (or more) daily by solely technician teams without a hair restoration surgeon’s involvement.
Such operations contrast sharply with the patient-centric, surgeon-led procedures that are the standard in more reputable clinics.
Such hair mill clinics, often focusing on quantity over quality, don’t provide the same level of care and expertise as surgeon-led clinics like Diamond Hair Clinic, where surgeon involvement is standard practice and operates just one patient a day.
This disparity in clinic practices underlines the importance of thorough research and consideration when choosing a clinic for such a delicate procedure.
We prefer not to mention the clinic’s name here to respect privacy and legal boundaries. However, the issue at hand needs to be addressed. Focusing on the patient’s concern rather than the specific clinic is essential.
What Is The Issue?
Two and a half months after the surgery, the patient reported an atypical hair shedding event. The patient provided photos depicting a shed hair graft containing 3 to 4 hairs, which is notably larger than the usual fine hairs typically lost during this phase. This finding is inconsistent with the normal post-surgical progression and necessitates further detailed examination.
Such a variance from the expected post-operative hair loss pattern indicates a possible anomaly in the patient’s healing and hair growth process. This unusual shedding was especially concerning as it occurred following hair combing.
This situation prompts a significant question in the patient’s mind: Is this a permanently lost hair graft?
Such questions are common and underscore the need for proper patient education on post-operative expectations.
To address this, it’s crucial to understand that shedding after hair transplant surgery is a normal part of the healing process. Shedding is a typical response of the hair follicles to the trauma of transplantation, but it can be alarming for patients who are not fully informed. Shedding is often mistaken for graft failure, a misconception that needs clarification.
In the initial weeks post-surgery, it’s common for transplanted hairs to fall out, a phase known as shedding or shock loss, paving the way for new hair growth.
During this phase, patients may observe what seems like an alarming amount of hair loss, but this is a typical and temporary phenomenon.
This is a natural reaction as the scalp adjusts to the trauma of transplantation. However, if the shedding includes a hair graft with multiple hairs, it warrants a more careful assessment.
Typically, what might appear as a lost graft is actually the shedding of the hair shafts while the follicle remains securely anchored under the scalp’s surface.
This distinction is crucial for understanding the healing process. That means that new hairs will likely grow from these follicles.
Though uncommon, a hair graft can be dislodged in the months following surgery, particularly if the scalp undergoes trauma or is exposed to excessive pressure. Such instances are rare but can occur due to various factors, including patient activity and post-operative care.
In this particular case, the patient’s experience of losing a graft with multiple hairs after two and a half months post-surgery is unusual but not necessarily indicative of permanent graft loss. This differentiation helps in assessing the true state of the transplant.
It’s important to differentiate between the normal shedding of dead follicles and the actual loss of grafts.
However, without in-person direct examination and more detailed information, it’s challenging to determine the nature of the shedding observed conclusively. A physical examination by a qualified hair transplant surgeon is indispensable in such cases.
The concern about shedding grafts, particularly ones that seem to contain multiple hairs, is a topic that merits further exploration. This case highlights the complexity of post-transplant care and the importance of continuous monitoring and guidance.
Understanding the Shedding and Hair Growth Cycle Post-Transplant
The Telogen Phase Post-Transplant
After a hair transplant surgery, the transplanted hair follicles typically enter the Telogen phase, a resting stage in the hair growth cycle.
The transition into the Telogen phase is a response to the physical intervention of transplantation and is a part of the body’s natural healing process.
The hair growth cycle consists of three stages: Anagen (Growth Phase), Catagen (Transition Phase), and Telogen (Resting Phase).
The surgical process, which involves the extraction and transplantation of hair follicles, as well as the effects of incisions and anesthesia, can cause the hair to transition into the Telogen phase.
In this phase, the follicles temporarily stop their growth activity, which is a standard response following the transplant procedure.
The Shedding Phase (Shock Loss)
After the hair transplant surgery, the newly implanted hair follicles, along with their attached hairs typically stay intact for about 1 to 3 weeks. This initial period of stability is followed by the natural shedding phase, which can be startling for patients.
It’s important to understand that this shedding is a normal part of the process and does not indicate that the body is rejecting the transplanted hair. Generally, around 3 to 6 weeks post-surgery, patients might undergo shedding, also known as “Shock Loss.”
Shock loss is a critical phase where the old hair makes way for new growth, indicating the start of the regenerative phase of the hair cycle. This term describes the loss of old hair from the follicles that have been transplanted.
Timeline for Regrowth
Shed hairs usually begin to regrow within a period of 3 to 12 months post-surgery. This timeline is vital for patient expectations, as hair regrowth is a gradual process and varies from patient to patient.
The ultimate outcomes, characterized by increased hair thickness, become more noticeable approximately 15 to 18 months after the procedure.
Biological Rationale for Shedding
Shedding is an accelerated response of the hair cycle due to the trauma experienced by the follicles during transplantation. The disruption caused by the surgical process triggers this shedding phase, which is an integral part of the hair’s natural cycle of renewal.
The disruption of the blood supply to the grafts temporarily leads to the loss of transplanted hair, a process essential for making way for new growth.
Medical Term – Effluvium
The medical term for this shedding phase is “Effluvium.”
Effluvium refers to accelerated hair shedding which can be seen in various conditions, including post-transplant scenarios. It typically involves hair shedding at the end of its lifespan, which can be hastened due to genetic balding patterns.
Native Hair Shedding and Regrowth
In addition to the shedding of transplanted hair, it is common for a patient’s existing-native hair to shed as well. This phenomenon may lead to an overall temporary decrease in hair density, which is a normal part of the transplantation process.
This is particularly true for hairs that are thin or miniaturized, often located amidst the newly implanted hairs.
Such shedding is a normal part of the process, with the expectation that the native hair will regrow. The regrowth of the native hair, along with the transplanted hair, contributes to the overall improvement in hair density post-transplant.
Therefore, shedding may encompass both the newly transplanted hair as well as the patient’s original hair in the transplanted region.
Hair Shedding in Donor Area
Although rare, especially under the care of an experienced hair restoration surgeon, shock loss in the donor area can occur but is typically temporary.
Patient Perception and Concerns
Shedding does not indicate damage to the hair grafts themselves. Understanding this can greatly alleviate patient concerns during the shedding phase. Even if a significant number of hairs are shed, this is part of the natural cycle, and the follicles remain intact.
During the shedding phase, the patient’s hair may appear thinner than usual. This temporary thinning is a visual effect of the shedding phase and should not be mistaken for a failed transplant. Although this can be a source of anxiety for the patient, it’s usually less noticeable to others.
Reassuring patients about the temporary nature of this thinning is an essential part of post-operative care. It’s important to reassure patients that this phase is temporary and a normal part of recovery.
Educating and Reassuring Patients
Educating patients about this natural cycle is crucial. Providing accurate and comprehensive information helps in building trust and managing patient expectations effectively.
Providing clear information and reassurance can significantly help manage their expectations and reduce undue stress or anxiety.
Differentiating Between Shedding and Graft Loss
Losing old dead hair shafts usually characterizes shedding and is typically characterized by a bulb at the end of the shed hair, which is the root sheath, not the growth center.
Graft loss, particularly the loss of an entire graft, is a less frequent but more significant concern in the initial stages following a hair transplant. During the first 72 hours post-procedure, the newly implanted hair grafts are at their most vulnerable to being dislodged.
Typically, if graft loss occurs, it happens within this critical 72-hour window. The dislodgement of grafts can often result from physical trauma. If it is accompanied by bleeding in the area where the graft was previously situated, this indicates graft loss.
The loss of a graft might be caused by physical trauma, such as accidentally bumping the head or unintentionally disturbing a scab, but this does not necessarily point to a larger problem with the transplant itself.
A hair graft consists of the 1-4 hair follicles and its necessary structures. If a patient notices a larger structure resembling a graft, it could be due to several factors, including improper graft handling during surgery or inadequate post-operative care.
However, such instances are rare when skilled and experienced hair transplant surgeons perform the surgery.
Further Complication Indicators
Apart from the loss of grafts, it’s important for patients to monitor for symptoms of infection or other complications. These include ongoing fever, significant bleeding, intense redness or pain, and the presence of green or yellow pus emanating from the scalp.
What Are Effective Methods to Reduce Shedding and Improve Graft Survival In Hair Transplant?
Minimizing shedding and enhancing graft survival in hair transplantation involves a multifaceted approach, combining pharmacological interventions and meticulous surgical planning.
Pharmacological Intervention with Finasteride and Dutasteride
Finasteride: It has been found that administering 1 mg of Finasteride daily, starting four weeks before and continuing up to 48 weeks after a hair transplant, can significantly improve scalp hair. This improvement is evident in the areas surrounding the hair transplant, thus enhancing the overall aesthetic outcome.
Finasteride achieves this by inhibiting the conversion of testosterone to dihydrotestosterone (DHT), which plays a key role in hair miniaturization and loss.
A study confirmed that finasteride treatment results in visible increases in superior/frontal scalp hair post-transplant compared to a placebo group.
Dutasteride: Similar to Finasteride, Dutasteride blocks the conversion of testosterone to DHT, but it is more potent. It inhibits both Type I and II 5-alpha reductase enzymes, with Type I enzymes also present in organs besides the skin. Dutasteride is approximately three times as potent as Finasteride at inhibiting the Type II enzyme.
A study comparing Dutasteride and Finasteride for male pattern hair loss showed that Dutasteride increased hair counts in a dose-dependent fashion and was superior to finasteride at improving scalp hair growth.
Surgical Planning and Execution
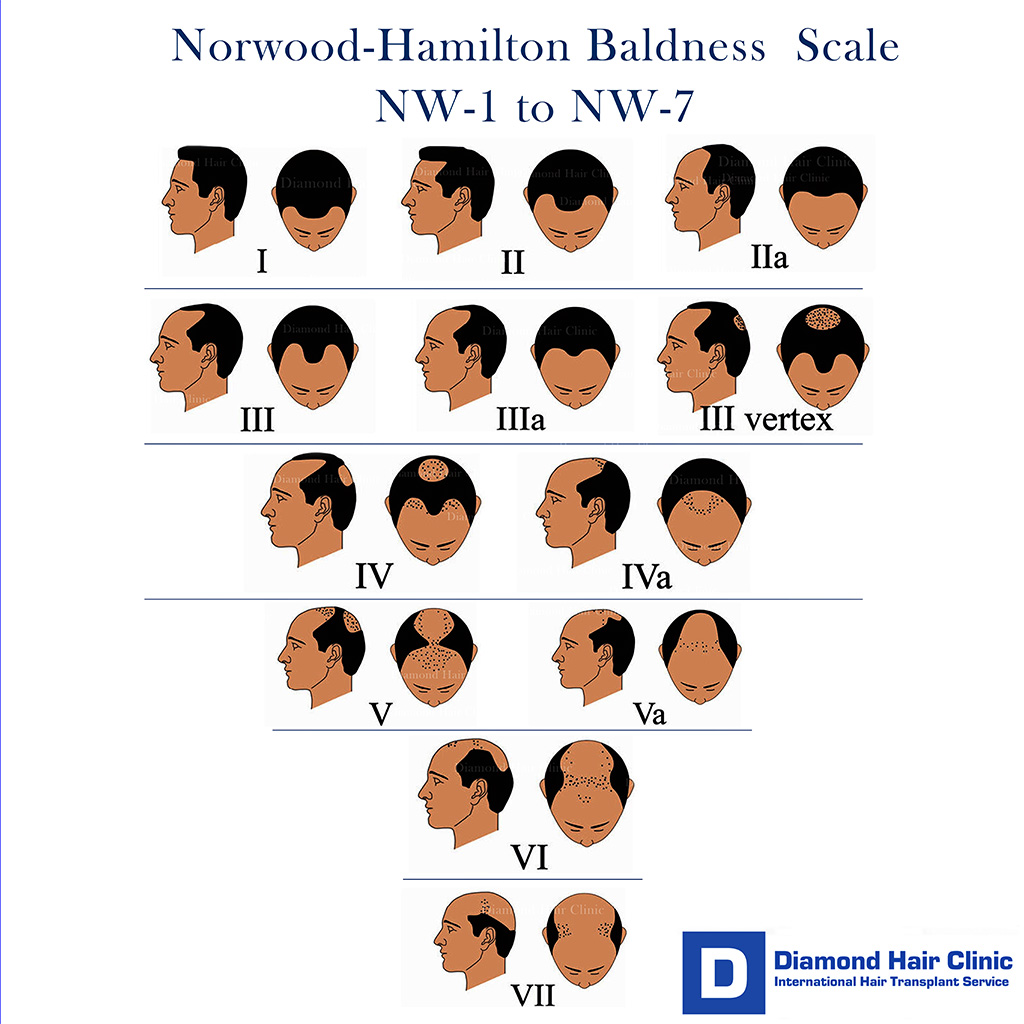
Determining the Number of Grafts: The number of grafts required for a hair transplant largely depends on the extent of hair loss, classified according to the Norwood Scale.
For example, a Norwood Class III pattern may require between 2000 to 2500 grafts, while a more advanced Class VII pattern may need 6000 to 7000 grafts.
The first session’s goal is to provide sufficient coverage and density so that the results appear natural and can stand on their own.
Goals of the First Session: The primary objectives include establishing or reinforcing the frontal hairline, providing coverage to thinning or bald areas, and adding sufficient density.
It is advised that the entire area requiring coverage be transplanted in one session rather than spreading it over multiple sessions. This approach not only expedites the process but also avoids repeated trauma to the donor site.
Timing of Subsequent Sessions: If a second session is desired, it should be considered only after the full growth of hair from the first session, typically 10 to 12 months.
This interval allows for assessment of the hair’s diameter, texture, length, and overall aesthetic, which can guide the placement of additional grafts.
Advantages of Large First Sessions: Performing a large procedure up to 4000 to 4500 hair grafts initially, particularly on a virgin scalp, offers several advantages. It enables easier placement of grafts due to intact skin elasticity and blood supply, maximizes the total yield of hair, and reduces the number of sessions needed.
This is important as each session can result in some loss of potential donor hair.
Addressing Shedding Risks: During hair transplant procedures, there’s a risk of shedding in the recipient area, particularly of hair that has started miniaturizing.
This emphasizes the need for substantial hair transplantation in areas with a high degree of miniaturization to ensure a cosmetically significant outcome.
Limitations in Graft Number: While the goal is to accomplish hair restoration quickly, there’s a limit to the number of grafts that can be transplanted in one session, ranging from 4000 to 4500 hair grafts.
High density of grafts increases the risk of vascular compromise and sub-optimal graft growth. Therefore, it’s crucial to balance the number and density of grafts to ensure the viability of the transplanted hair.
Challenges of Mega Sessions: Large-scale transplant sessions require extensive planning and resources. Factors like the time grafts remain outside the body, the need for more surgical staff, and patient fatigue must be considered.
Additionally, the size of the hair grafts and the recipient sites is crucial, as larger sites can cause more damage to the blood supply, limiting the number of grafts that can be placed at one time.
A combination of pre and post-operative pharmacological treatment with Finasteride or Dutasteride and strategic surgical planning, including determining the appropriate number of grafts and timing of sessions, is essential in minimizing shedding and enhancing graft survival in hair transplantation.
This approach addresses both the biological factors of hair loss and the technical aspects of the transplantation process.
Patient-Specific Factors for Shedding: The healing and shedding process can vary significantly among individuals. Factors such as the patient’s age, health, scalp condition, and lifestyle choices can influence the rate and nature of hair shedding and regrowth.
Each patient’s experience can vary. Some patients may not shed at all, while others may notice shedding of the transplanted hair or their original hair in the transplant area, which can make the area temporarily appear thinner.
The Importance of Post-Operative Care
Adhering to post-operative care instructions is critical. Patients should avoid harsh chemicals, excessive heat or cold, and physical trauma to the scalp. Gentle handling of the hair and scalp, especially in the first few months, is essential.
Consultation with Your Surgeon
If there are concerns about unusual shedding or graft loss, immediate consultation with the surgeon who operated on you is advised. This step addresses potential issues and mental peace and sets realistic expectations about the hair growth process.
Post-operative shedding is a common and expected phase in the hair transplant recovery process. This stage, while sometimes alarming to patients, is a natural part of the hair’s growth cycle.
Understanding this and how personal factors might influence recovery can empower patients during their post-transplant period.
Every patient experiences a unique healing journey. Regular consultations with the hair transplant surgeon are vital for personalized guidance and reassurance, ensuring that the patient’s recovery aligns with the desired successful outcomes of the hair restoration surgery.